
The Capacity Estimator (CapEs) project was designed to see if we can estimate the primary care capacity of a team of health care providers and how closely that might meet the primary care needs of a population of people.
It began as a spreadsheet (that was never used) and then, a few years ago, we re-designed it as a dynamics simulation model.
The first versions have been used in BC to support planning of primary care networks and several clinic proposals. It included family physicians, nurse practitioners, and nurses. There was limited evidence for the capacity and amount of shared care that could happen between different care providers. That led us to our CapEs Grant.
CapEs Grant

Recognizing that there is a health human resources and capacity crisis in Canada and that many provinces are looking at team based care as a potential solution in primary care, we wanted to expand the evidence for capacity gains of registered nurses and allied health professionals in primary care. Given the lack of evidence in Canada, we decided to start with a series of modified Delphi processes to collect expert opinion on capacity and shared care of several common healthcare professional groups being hired into primary care.
The CapEs study evidence could then be shared and also incorporated into the CapEs simulation software to better help predict how primary care capacity can be changed with team-based care.
This study is funded by the Canadian Institutes of Health Research (CIHR).
Grant Goals
- Co-develop and validate the evidence of how registered nurses and allied health providers add capacity to a primary care team;
- Translate that newly synthesized evidence into the CapEs web application; and
- Share the CapEs web application with primary care planners and decision makers in multiple provinces to support team-based care planning.
Study Approach
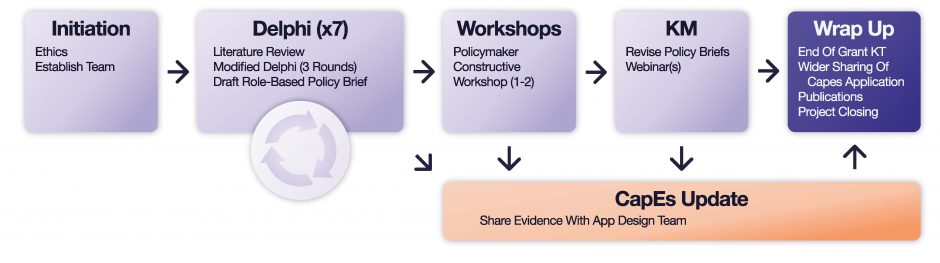
From July 2023 to April 2024 we engaged with stakeholders to co-develop capacity estimations for the following primary care roles: registered nurses (RN), clinical pharmacists (CP), physician assistants (PA), social workers (SW), registered dietitians (RD), physiotherapists (PT), occupational therapists (OT).
We used a combination of literature scans and online modified Delphi processes to co-develop and validate the evidence for each primary care role. The Delphi process is a research method that uses experts’ opinions about a topic by asking structured questions in an anonymous survey format. The goal is to reach consensus.
Each CapEs Delphi process consisted of three rounds of survey questions with a panel of ten experts. The answers from each round were processed by the research team and the questions were re-formatted and sent out again, in iterations, until consensus was reached.
Findings
Early findings on Nurses in Primary Care were shared with the Ministry of Health and used to inform the Nurse Compass project, which we developed in collaboration with Health Quality BC.
Policy Briefs
Draft policy briefs were developed for each profession using the findings from the literature and Delphi processes. These policy briefs are available to download for each individual profession or as a package for all professions:
- All professions
- Registered nurses
- Clinical pharmacists
- Physician assistants
- Social workers
- Registered dietitians
- Physiotherapists
- Occupational therapists
CapEs Software – Release 3
We have revised the CapEs software in release 3 with the information from the study and have started using this as a tool to help communities and clinics explore the primary care needs and how they might be addressed.
Below are two screenshots of the software showing a simple solo doctor’s office (left) and a larger and more complex team (right). You can see how the CapEs software tries to estimate how the primary care needs are prioritized through the simulation and the user gets a summary of that estimation in the graphs.


Next Steps
We are now expanding CapEs work to explore how different roles uniquely support equity deserving populations in primary care.